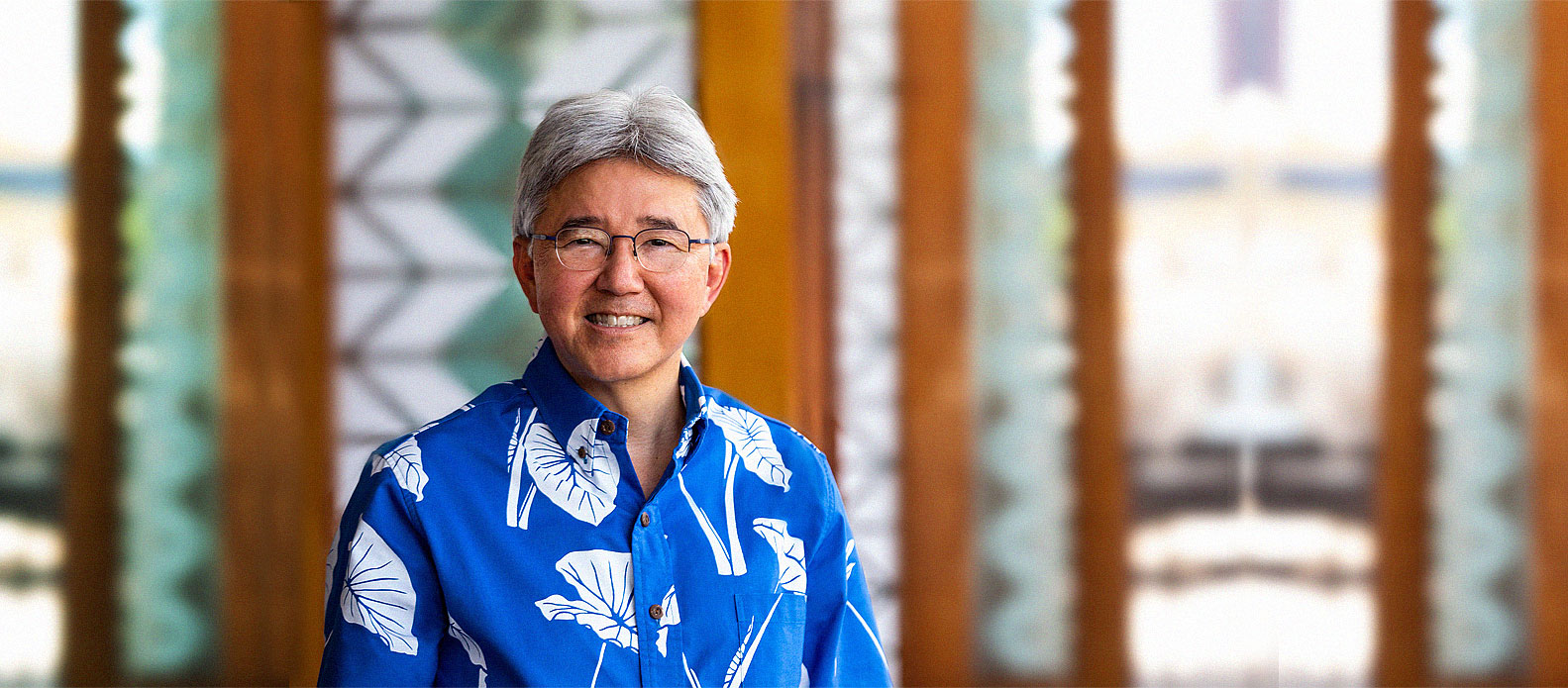
In an industry ripe for innovation and visionary leadership, Ray Vara is poised to guide Hawai‘i through a time of great change as the forward-thinking leader of the largest healthcare system in the state. Prior to joining Hawai‘i Pacific Health in 2002, Vara was CEO of New Mexico’s Los Alamos Medical Center and held leadership positions at several U.S. Army medical facilities on the mainland. His responsibilities now include executive oversight of Straub Medical Center, Kapi‘olani Medical Center for Women & Children, Pali Momi Medical Center and Wilcox Health on Kaua‘i. Read on for his take on the state of the healthcare industry and the role Hawai‘i Pacific Health is playing in shaping the future of our nation’s health.
What is the greatest obstacle facing the healthcare industry in Hawai‘i?
It’s no secret that healthcare costs are a significant issue in this country. Right now they represent about 18 percent of the gross domestic product. Based on the last projections I’ve seen, that number will be about 38 percent by 2050. We’d bankrupt the country long before we get there.
It’s clear there’s a vital need for transformation from a fee-for-service environment, where payment is on a per-unit basis, to a more value-based system, where we get paid for providing higher quality of care and creating a healthier population.
There’s a Grand Canyon between those two systems, and you have make a very deliberate decision about when you’re going to make that transition between the two. I think the challenge that every healthcare system in the country is facing is how to bridge that gap.
To be clear, I’m not saying we’re going to lower the cost of healthcare, but I do think we can bend the cost curve by transitioning to a more value-based system, and that’s done by providing higher quality of care and reaching deeper into our communities to address the social determinants of health beyond the care that we can provide within our facilities.
What specific challenges are involved in making that transition?
We know, for example, that people often end up in the emergency room when they don’t have a primary care physician or because they’re not getting routine care on a preventative and proactive basis. While emergency rooms serve a critical need in our communities, it’s not the most efficient form of primary care. We believe there are more effective ways to get patients access to other portals of entry.
Emergency rooms are one of the higher cost-of-care environments because they have to do a full assessment of every patient who comes in. It’s not only less costly to help patients find a primary care provider, it also means better quality of care over the long run because they can develop a relationship with a healthcare provider on an ongoing basis.
That being said, emergency rooms are a good revenue source for hospitals, so before you transition to that less costly care environment, you have to make sure there’s a way to get there that allows the system to sustain itself. What we’re trying to do is figure out how to transition to a more value-based system that offers patients the very best care and allows the revenue stream to support the transition.
How would you describe Hawai‘i Pacific Health’s approach to effecting change?
At Hawai‘i Pacific Health we have an annual gathering of our boards where we set strategy. The most recent one had to do with challenging the norms of traditional healthcare systems and processes. We’re not going to make progress by doing things the way we do them now.
Past themes have addressed unprecedented collaboration and fostering a willingness to intentionally disrupt the system and think beyond what we’ve ever thought possible. We then empower our leaders to deliver those strategies throughout the organization.
Hawai‘i Pacific Health is neck and neck for being the largest nongovernmental employer in the state. How do you keep such a large body of employees engaged?
Setting a mission statement as bold as creating a healthier Hawai‘i requires building and maintaining a phenomenal team. We need a cadre of people who are 100 percent committed to their mission and who are passionate about it, which also means we have to be a great employer.
We have to build that passion, empower our employees and make sure they know they’re part of something bigger than themselves and that they are making a great impact in our community. When you have 7,000 people, and you consider their families and all the people they touch, I think we make a pretty broad impact from an employer standpoint.
We perform what many would consider miracles on a daily basis. Earlier today I was walking around Kapi‘olani, where a baby was born just over one pound. We have every reason to believe we’ll be able to nurse that baby to health. That wasn’t possible not so many years ago. Whether you are a physician, nurse or member of our support staff, it’s important that everyone knows they are part of that effort.
What are some of the biggest turning points in healthcare that you’ve observed over the course of your career?
The electronic medical record comes to mind. It’s allowed us to do a lot of things in terms of advancing the integration of healthcare, improving quality and joining all of our providers across the system together in a meaningful way.
The difference between what I would call the managed care of the past and global capitation of the future is that now we have data. We can look at individual patient outcomes as well as population-wide outcomes. We’re constantly looking at the data for our population base in very specific areas where we see opportunities to make improvements in the health of our community.
How has that process been?
We were early adopters of the electronic medical record, so it came with a lot of change in the organization. But we did it very deliberately, and I think the way we went about it was the right way versus taking a big-bang approach.
We’ve received a lot of recognition for the progress we’ve made. The Davies Award is the highest national award you can receive for successfully utilizing health information technology from a patient-impact standpoint. We received the award twice, in 2013 and 2016. There’s only one other system in the country that can say that.
In what ways is Hawai‘i Pacific Health disrupting the current healthcare landscape?
Besides early deployment of the electronic medical record, I would say our primary care expansion strategy. We currently have a number of clinics under construction or expansion throughout the islands. Our intent is to add 50 new primary care physicians to Hawai‘i Health Partners, our accountable care organization, over the next five years in order to serve what I believe to be the greatest need in healthcare—a shortage of primary care.
Specialists account for a greater share of the healthcare dollar than primary care physicians. Is that something Hawai‘i pacific Health is looking to shift?
Specialists play a critical role in the fabric of the healthcare system and that’s always going to be the case. The shift is going to come about by being more proactive about care management and providing higher quality of care. In that respect, we see the primary care physician playing a greater role within our system and the community.
What are your thoughts on the direction and evolution of the Affordable Care Act?
I recently participated in a discussion on this specific topic in the Catalyst version of the New England Journal of Medicine with a number of others, including Dr. Don Berwick, President Obama’s former Center for Medicare and Medicaid Services administrator. The whole policy discussion, frankly, can be a lot of noise. There’s always going to be a lot of activity and changes around policy with different administrations and the way those policies roll out, and we’re going to be subject to those policies.
We haven’t allowed it to distract us from the work we have to do at Hawai‘i Pacific Health. We know that healthcare in this country has to change, we know that the trajectory of healthcare costs has to change, and we know it’s going to be done through partnership between providers, payers and communities. We don’t spend a lot of time and energy worrying about policy because we know what has to be done and we’re laser focused on that effort via Hawai‘i Health Partners, an organization made up of our four hospitals and 900 employed and independent physicians, which will serve as the vehicle to see it through.
To what extent are other organizations around the country doing this?
There are a number of providers around the country that have tried to do it without a payer or health plan partner, but from a financial standpoint, they have to figure out how to get paid to do that work. As with adoption of the electronic medical record, we’re truly at the tip of that spear.
With HMSA as a payer, we have among the most innovative partnerships of anywhere in the country. Further, our quality of care, patient satisfaction and employee-engagement data is on par with that of the nation’s best healthcare systems. It’s just a matter of continuing that transformational effort over the coming years.
Amazon, Berkshire Hathaway and JPMorgan Chase have formed a partnership to overhaul the deployment of healthcare for their employees. What are the implications of non-healthcare corporations entering the market?
I think time will tell. The fact that those outside the industry are getting impatient to see progress is certainly a nudge for those of us within the industry. Too much of the healthcare industry has been waiting on policy to guide us down the path rather than taking our own initiative. In that sense, I think it’s a good thing. It’s a good stimulus for our industry to get to work.